Testicular Cancer Tests: The Pathology Report
After the orchiectomy, the removed testicle and spermatic cord are sent
to the pathology lab where they are evaluated by a pathologist. Once finished,
the pathologist will create a report describing the specimen and findings.
The pathology report is very important because the treatment plan
is based on the pathologist's observations.
In the case of testicular cancer, you must be aware that pathologists
are no different from general practitioners, urologists, or oncologists, and the pathology report is usually an opinion, not a hard fact.
Testicular cancer is relatively rare, and chances are pretty good that
a normal pathologist does not get to see testicular tumors more than a
couple of times a year, if that. If your cancer is unusual or your
treatment is highly dependent on the pathology report, then it probably
is a good idea to get a second opinion from the pathology department
at a referral center that sees testicular cancer frequently. Some
pathologists that fall into this category can be
found on our experts list. Some specific instances
where a second opinion is advised are:
- Men under 30 diagnosed with pure seminoma who are considering radiation therapy.
- Men diagnosed with Stage I nonseminoma who are considering surveillance.
- Men diagnosed with any benign tumor such as a mature teratoma or a dermoid cyst.
- Men diagnosed with a stromal cell tumor such as a Leydig or Sertoli cell tumor.
- Men diagnosed with any non-germ cell elements in their tumor such as Rhabdomyosarcoma,
Leiomyosarcoma, PNET, Lymphoma, Leukemia, etc.

In our opinion, the pathology report on a testicular germ cell tumor
should include the following information1:
-
Tumor type: The histologic type of tumor present. If the tumor is
a mixed germ cell cancer, the components in the tumor should be listed
in order of relative abundance. The pathologist should attempt to give
a numeric estimate of the percentages of each element, especially when
one of the elements is embryonal carcinoma. This percentage is particularly
important for men considering surveillance. It is thought that the more
embryonal carcinoma there is in the tumor, the more likely that the cancer
has spread beyond the testicle.
- Staging information: The size and appearance of the tumor should
be listed. Local spread--into the rete testis,
tunica albuginea, epididymis,
and spermatic cord--should also be listed. If the cord is involved, the
report should indicate if any cancer was found at the surgical margin (the
point where the cord was cut).
-
Vascular/Lymphatic invasion: The tumor should be assessed for presence
or absence of vascular or lymphatic invasion. This is also very important
for men considering surveillance. The presence of vascular invasion indicates
a greater likelihood that the cancer has spread beyond the testicle.
-
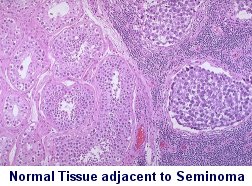
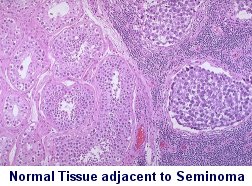
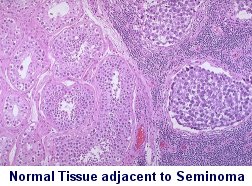
Status of the remainder of the testis: Evidence of cryptorchidism
or other developmental abnormalities should be mentioned. Such features
may imply a greater risk for the development of a tumor in the remaining testicle.
Also, if possible, the presence of normal spermatogenesis elsewhere
in the uninvolved testis should be reported. This finding may suggest a
relatively decreased risk for cancer in the remaining testicle and is a
likely indicator of fertility should the patient consider sperm banking
prior to retroperitoneal surgery and chemotherapy. The finding of mature
sperm in the epididymis is an easy way to confirm that the testicle was still producing sperm in spite of the tumor.
-
Incidental findings: Lipomas or hydroceles of the cord, adrenal
rests, and spermatoceles or other cysts may be found. Epididymitis may
also be noted.
Review the pathology report with your doctor, and get a copy of it. If you do
not understand any part of it, be sure to get an explanation from the doctor. If
you think, based on what you read here, that information is missing, be sure
the doctor knows. He can always ask the pathologist to review the slides again. The
slides are not thrown away. They are probably kept by the hospital on the order
of 7 years, so they are available for another look if that becomes important.
While not a part of the routine pathology report, other investigational
items may be used at some time in the future. The genetic isochrome 12 [i(12)p]
may be used to prove the germ cell origin of extragonadal tumors that are
otherwise hard to identify. Some researchers2
have proposed the use of the immunohistochemical expression of Ki-67 to
predict which Stage I non-seminoma patients should have an RPLND. However,
it has not proved itself to be useful as of yet, and other researchers
doubt its efficacy.3
Relevant Links:
References
-
Brodsky, G.L. "Pathology of Testicular Germ Cell Tumors,"
Hematology/Oncology Clinics of North America, Vol. 5(6), 1991.
-
Albers P, Bierhoff E, Neu D, Fimmers R, Wernert N, Müller
SC. MIB-1 immunohistochemistry in clinical stage I nonseminomatous testicular
germ cell tumors predicts patients at low risk for metastasis. Cancer
Vol 79(9),1997;1710-6.
-
Heidenreich A, Sesterhenn IA, Moul JW. Prognostic risk
factors in low stage testicular germ cell tumors. Cancer Vol 79(9),1997;1641-5.
Click on this to go back to the TCRC main page:

This page was last updated on
Mar 28, 2018