Testicular Cancer Info: Staging
What is Staging?
Once testicular cancer has been diagnosed, the doctor will perform more tests to determine whether the cancer has spread from the testicle to other parts of the body. Classifying a person's cancer by the degree to which it has spread is called staging. Staging is used to determine the available treatment options. Keep in mind that staging is only as accurate as the information available, and the stage of a person's cancer can change as more information or more accurate information is gathered. If the doctor comes out of the operating room and tells you he thinks he got it all, don't be so quick to believe him. It takes urologists, pathologists and radiologists to ultimately determine the stage of the cancer.
There are two type of staging: Clinical and Pathological. Clinical staging uses radiological and physical clues to estimate the stage. Pathological staging uses stronger evidence like tissue samples and blood tests to determine the stage. For example, assume you have gone through the orchiectomy and based on all the test results, your doctor says that you have Clinical Stage I Nonseminoma. At this point you choose to have an RPLND. If they find no cancer during the RPLND, they will change you to Pathological Stage I. If they do find cancer, then you will become Pathological Stage II. As you can see, the Pathological Stage is more accurate since it used actual tissue samples to determine the presence or absence of cancer.
Tests & Procedures
It is one thing for the doctor to do a physical exam and conclude that you probably have cancer. It is another thing to determine the stage. Usually the stage cannot be estimated until after surgery, blood tests and xrays have been done. Here is a list of tests that may be used to determine the stage:
Surgery: Without surgery, in this case an orchiectomy, it is often difficult to conclude that there is cancer there at all, so surgery is usually the first step.
Blood tests: Some testicular cancers secrete something called tumor markers, high levels of certain proteins that can be detected through blood tests. These markers of testicular cancer include alpha-fetoprotein (AFP), beta human chorionic gonadotropin (ß-HCG) and lactate dehydrogenase (LDH). If a guy's AFP or HCG level are above normal AND there is something wrong with his testicle, then you can assume that he has testicular cancer. If the tumor markers do not fall back to normal after an orchiectomy, then you can usually assume that the cancer has spread, even if no other tests show where it has gone. For more information on tumor markers, click here.
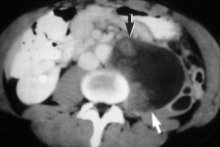
Computed Tomography (CT) scanning: This machine uses a rotating X-ray beam to create a series of pictures of the body from many different angles. A computer processes the information and produces a detailed cross-sectional image of selected parts of the body. Sometimes, a dye is injected into a vein to highlight details on the scan. A CT scan is especially valuable for identifying the spread of tumors to lymph nodes. If the tumor markers are high enough, a CT scan may also be done of the brain. Keep in mind, however, that it is hard to see into areas like the abdomen, and just because a CT scan says everything is normal does not mean that the cancer has not spread at all.
Chest X-rays: Simple chest x-rays are often used to determine if the cancer has spread to the lungs. In many cases the doctor will order a CT scan of the chest right after cancer has been diagnosed just to be sure nothing is there. (CT scans can see smaller masses in the lungs than chest x-rays, but in many cases these masses are not tumors.)
Positron Emission Tomography (PET): PET scanning is a relatively new technology that allows doctors to view biological functions. Areas with increased metabolic activity show up as "hot areas" in a PET image. Instead of using an x-ray, they give you a radioactive substance and use the scanner to try to detect where that radioactive material is collecting in the body. The theory is that the radioactive material is more likely to go to solid tumors than other areas of the body. Its use is promising in the future, particularly in evaluating large masses left over after chemotherapy for seminoma. However, at this time it is still experimental, expensive, hard to interpret, not widely available and probably should not be used in staging.
Magnetic Resonance Imaging (MRI): An MRI uses magnetic fields and radio waves to create images of selected areas of the body. These images can show enlarged lymph nodes and abnormal growths in certain organs that may indicate that the cancer has spread. MRI's are typically not used with testicular cancer because the CT scan often produces a better result and costs less.
Lymphangiography: This painful test involves injecting a special radioactive dye into the lymphatic system. Over a period of several hours, the dye collects in areas where cells are dividing and growing quickly. The doctor takes an X-ray, which shows where the dye has gathered and where cancer might be found. This test used to be performed to map out the lymph nodes in the retroperitoneum so the radiation fields could be set up to treat a patient with seminoma tumors. It is rarely used any more because it is not particularly accurate, and it almost certainly is not used for staging. It is a good bet that your doctor is getting on in years if they order this test.
Stages of testicular cancer
After the required testing has been done, the doctors can assign a stage to your cancer. Roughly speaking, here are the Stages used:
- Stage I: Cancer is found only in the testicle. Removing the testicle alone should cure the patient, though many will choose some form of additional treatment just to be sure...
- Stage II: Cancer has spread to the lymph nodes in the abdomen. Removing the testicle alone will not cure the patient, and more treatment is necessary.
- Stage III: Cancer has spread to areas above the diaphragm such as the lungs, neck or brain. There may be also be cancer in parts of the body such as the bones or liver. In this situation, chemotherapy is absolutely required. Surgery may also be needed.
- Stage IV: To the best of my knowledge, there is no such thing as Stage IV testicular cancer. However, it is possible that Stage IV may still be used in some places in Europe. Suffice to say that Stage IV is probably very similar to Stage III.
- Recurrent: Recurrent disease means that the cancer has come back after it has been treated. It may recur in the same place or in another part of the body.
In reality, however, there are many subclasses as well, so it can get kind of complicated. What follows is the complete TNM Staging Protocol used by most doctors in the world today, as defined by the American Joint Committee on Cancer (AJCC). [1]
TNM definitions
Primary tumor (T) - The extent of primary tumor is classified after radical orchiectomy.
- pTX: Primary tumor cannot be assessed (if no radical orchiectomy has been performed, TX is used.)
- pT0: No evidence of primary tumor (e.g., histologic scar in testis)
- pTis: Intratubular germ cell neoplasia (carcinoma in situ)
- pT1: Tumor limited to testis and epididymis without lymphatic/vascular invasion
- pT2: Tumor limited to testis and epididymis with vascular/lymphatic invasion, or tumor extending through the tunica albuginea with involvement of the tunica vaginalis
- pT3: Tumor invades the spermatic cord with or without vascular/lymphatic invasion
- pT4: Tumor invades the scrotum with or without vascular/lymphatic invasion
Regional lymph nodes (N)
- NX: Regional lymph nodes cannot be assessed
- N0: No regional lymph node metastasis
- N1: Metastasis in a single lymph node, 2 cm or less in greatest dimension
- N2: Metastasis in a single lymph node, more than 2 cm but not more than 5 cm in greatest dimension; or multiple lymph nodes, none more than 5 cm in greatest dimension
- N3: Metastasis in a lymph node more than 5 cm in greatest dimension
Distant metastasis (M)
- MX: Presence of distant metastasis cannot be assessed
- M0: No distant metastasis
- M1: Distant metastasis
- M1a: Non-regional nodal or pulmonary metastasis
- M1b: Distant metastasis other than to non-regional nodes and lungs
Serum tumor markers (S)
- SX: Tumor marker studies not available or not performed
- S0: Tumor marker levels within normal limits
- S1: LDH < 1.5 X Normal and HCG (mIu/ml) < 5000 and AFP (ug/ml) < 1000
- S2: LDH 1.5-10 X Normal or HCG (mIu/ml) 5000-50,000 or AFP (ug/ml) 1000-10,000
- S3: LDH > 10 X Normal or HCG (mIu/ml) > 50,000 or AFP (ug/ml) > 10,000
| Stage 0
pTis, N0, M0, S0
|
Stage I
pT1-4, N0, M0, SX
Stage IA
pT1, N0, M0, S0
Stage IB
pT2, N0, M0, S0
pT3, N0, M0, S0
pT4, N0, M0, S0
Stage IS
Any pT/Tx, N0, M0, S1-3
|
Stage II
Any pT/Tx, N1-3, M0, SX
Stage IIA
Any pT/Tx, N1, M0, S0
Any pT/Tx, N1, M0, S1
Stage IIB
Any pT/Tx, N2, M0, S0
Any pT/Tx, N2, M0, S1
Stage IIC
Any pT/Tx, N3, M0, S0
Any pT/Tx, N3, M0, S1
|
Stage III
Any pT/Tx, Any N, M1, SX
Stage IIIA
Any pT/Tx, Any N, M1a, S0
Any pT/Tx, Any N, M1a, S1
Stage IIIB
Any pT/Tx, N1-3, M0, S2
Any pT/Tx, Any N, M1a, S2
Stage IIIC
Any pT/Tx, N1-3, M0, S3
Any pT/Tx, Any N, M1a, S3
Any pT/Tx, Any N, M1b, Any S
|
In addition to the clinical stage definitions, surgical stage may be designated
based on the results of surgical removal and microscopic examination of tissue.
Stage I
- Stage I testicular cancer is limited to the testis. Invasion of the scrotal
wall by tumor or interruption of the scrotal wall by previous surgery does not
change the stage but does increase the risk of spread to the inguinal lymph
nodes, and this must be considered in treatment and follow-up. Invasion of the
epididymis tunica albuginea and/or the spermatic cord also does not change the
stage but does increase the risk of retroperitoneal nodal involvement and the
risk of recurrence. This stage corresponds to AJCC stages I and II.
Stage II
- Stage II testicular cancer involves the testis and the retroperitoneal or
para-aortic lymph nodes usually in the region of the kidney. Retroperitoneal
involvement should be further characterized by the number of nodes involved and
the size of involved nodes. The risk of recurrence is increased if more than 5
nodes are involved, if the size of 1 or more involved nodes is larger than 2
centimeters, or if there is extranodal fat involvement. Bulky stage II disease
describes patients with extensive retroperitoneal nodes (>5 centimeters) who
require primary chemotherapy and who have a less favorable prognosis. This
stage corresponds to AJCC stages III and IV (no distant metastasis).
Stage III
- Stage III implies spread beyond the retroperitoneal nodes based on physical
examination, x-rays, and/or blood tests. Stage III is subdivided into nonbulky
stage III versus bulky stage III. In nonbulky stage III, metastases are
limited to lymph nodes and lung with no mass larger than 2 centimeters in
diameter. Bulky stage III includes extensive retroperitoneal nodal
involvement, plus lung nodules or spread to other organs such as liver or
brain. This stage corresponds to AJCC stage IV (distant metastasis).
As if all that staging information wasn't enough to confuse you, the experts decided to classify testicular cancer patients in yet another way: according to risk. In many cancers you can determine how bad the cancer is by looking at the staging information. With testicular cancer, it isn't often that simple. You may have stage III cancer and be more likely to be cured than someone else with stage II cancer. The following table breaks up patients into good, intermediate and poor risk categories using tumor markers, pathology, and location of any metastatic tumors.
|
|
|
Risk
|
Seminomatous tumors
|
Nonseminomatous tumors
|
|
|
Good |
Any primary site
and
No nonpulmonary visceral metastasis
and
Normal AFP,
any hCG,
any LDH level
|
Testicular or retroperitoneal primary tumor
and
No nonpulmonary visceral metastasis
and
Good markers (all of the following):
AFP <1,000 ng/mL
hCG <5,000 mIU/mL
LDH <1.5 x ULN
|
|
|
Intermediate
|
Any primary site
and
Nonpulmonary visceral metastasis
and
Normal AFP,
any hCG,
any LDH level
|
Testicular or retroperitoneal primary tumor
and
No nonpulmonary visceral metastasis
and
Intermediate markers (any of the following):
AFP 1,000-10,000 ng/mL
hCG 5,000-50,000 mIU/mL
LDH 1.5-10 x ULN
|
|
|
Poor
|
None
|
Mediastinal primary tumor
or
Nonpulmonary visceral metastasis
(brain, liver, bone, etc.)
or
Poor markers (any of the following):
AFP >10,000 ng/mL
hCG >50,000 mIU/mL
LDH >10 x ULN
|
|
|
AFP, alpha-fetoprotein; hCG, human chorionic gonadotropin; LDH, lactate dehydrogenase; ULN, upper limit of normal.
Adapted from International Germ Cell Cancer Collaborative Group |
References:
- Testis. In: American Joint Committee on Cancer: AJCC Cancer Staging
Manual. Philadelphia, Pa: Lippincott-Raven Publishers, 5th ed., 1997, pp
225-230.
Click on this to go back to the TCRC main page:

This page was last updated on
Mar 29, 2018